Knowledge Center
Everything You Need to Know About Fertility Options…But Were Afraid to Ask!
In Vitro Fertilization (IVF) FAQ
Q: What is In Vitro Fertilization (IVF)?
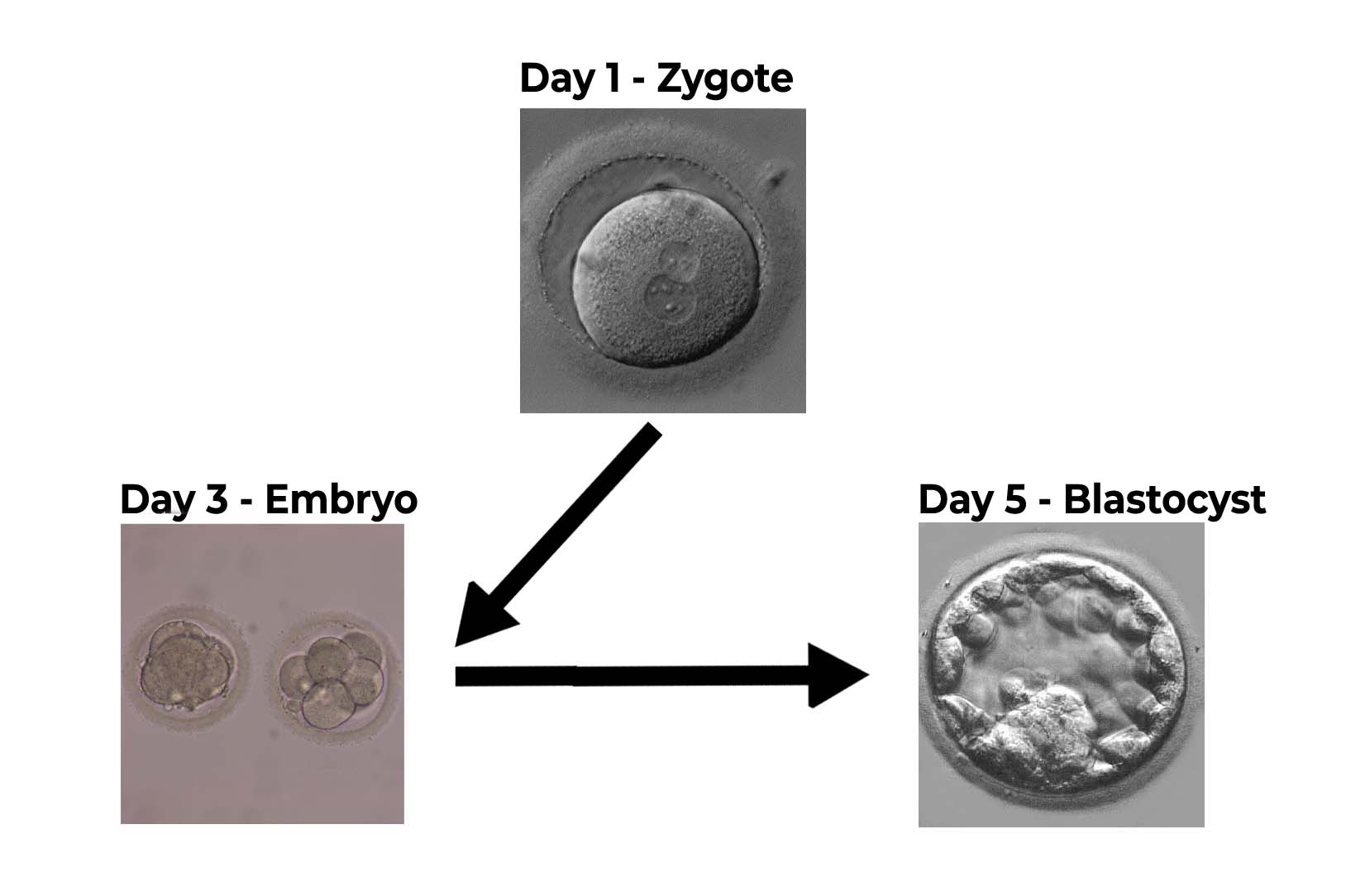
A: In Vitro Fertilization (IVF) is a type of assisted reproductive procedure used for infertility treatment. To perform IVF, female eggs are fertilized with the male partners or (sperm donor) in the laboratory. The resulting embryos from this process are transferred into the female partner’s uterus (womb). Typically, the created embryo(s) are grown and cultured in the lab for 3-5 days.
Q: What are the Advantages of In Vitro Fertilization?
Another great advantage of IVF is that it can be used to make specific diagnoses. Since the embryo is created in the lab it gives physicians the ability to test the embryos for any genetic or chromosomal abnormalities. IVF therefore can be used to diagnose inheritable diseases. Some of the most common diseases tested are cystic fibrosis, sickle cell disease, and chromosomal abnormalities such as Down Syndrome and Turner Syndrome.
Finally, IVF has the highest success rate in achieving a pregnancy for couples. It also affords couples the option to store and freeze extra embryos that are created for future fertility.
Q: How long is an IVF Cycle?
A: An IVF cycle normally lasts about a month, very similar to a regular reproductive cycle. Day 1 starts at the first day of menstrual bleeding. Most egg collections occur around the 12-14th day of an IVF cycle. But it may vary individually, from patient to patient, and from cycle to cycle.
On the day of the egg collection, the egg is exposed to sperm (IVF) or a single sperm is injected into the egg (ICSI). The embryo transfer will be performed 3-5 days later. And pregnancy test will be performed two weeks after the egg collection. Some clinics utilize oral contraceptives to control the period to ensure the patients going through treatment are right on schedule.
Q: What is the difference between a day 3 and day 5 Embryo transfer?
A: Eggs that are fertilized successfully are transferred into culture media to promote the growth of the now newly formed embryo. Embryos are generally transferred on day 3 or 5 of embryo development. The day of transfer depends on embryo number, quality, patient characteristics, and laboratory practices. Patients should discuss thoroughly the benefits and disadvantages of day 3 or day 5 transfers.
Most embryo transfers at ARC are day number 5 (Blastocysts). Blastocysts have higher success and are more likely to implant. At ARC, your embryos are transferred at the blastocyst stage to lower multiple births specially if tested for aneuploidy with PGT-A.
Q: What if my eggs don’t fertilize?
Intrauterine Insemination (IUI) FAQ
Q: What is Intrauterine Insemination (IUI)?
Q: Who should consider IUI?
A: An IUI procedure can be helpful in several situations including mild male factor infertility, cervical or cervical mucous concerns, unexplained infertility, mild endometriosis, individuals, or couples using donor sperm; and women with ovulation conditions who have responded well to fertility medications.
Q: How much does intrauterine insemination cost?
Q: What is the difference between IUI & IVF?
A: The key difference between IUI and IVF is that IUI involves fertilization inside the uterus and with IVF, fertilization takes place outside of the body in the laboratory. During IVF, an individual takes fertility medication to stimulate then ovaries and then the mature eggs are retrieved during a minor surgical procedure. The eggs are the fertilized in the lab with prepared sperm. The resulting embryos can then be transferred to the uterus, or frozen for later use.
Q: What are the risks of IUI?
A: IUI is a low-risk procedure, but there are some concerns to be aware of. These can include:
- Infection
- Becoming pregnant with twins/multiples
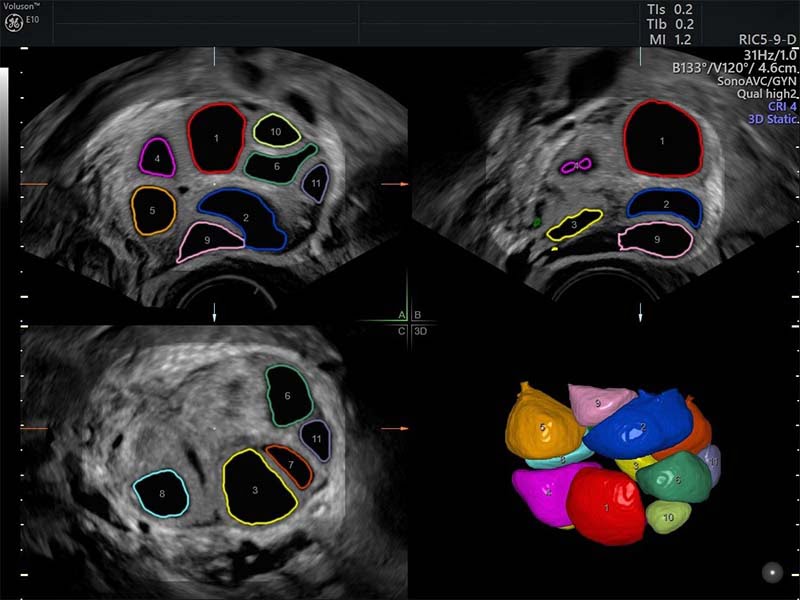
Our experienced and board-certified reproductive endocrinologist closely monitors your cycles with blood work and ultrasounds. Monitoring your cycles requires extensive training and experience to avoid multiple pregnancies (triplets, etc.)
Preimplantation Genetic Testing/Diagnosis (PGS/PGD) FAQ
Q: What is preimplantation genetic testing (PGT)?
Q: Are there different types of genetic testing?
A: Yes. There are three types of PGT:
Preimplantation genetic testing for aneuploidy (PGT-A): This type of PGT screens embryos for certain types of chromosome abnormalities. Human embryos should have 23 pairs of chromosomes in each cell. One chromosome in each pair is contributed by the egg, and the other is contributed by the sperm. It is common for embryos to have random chromosome abnormalities such as a missing or extra chromosome (aneuploidy). These chromosome abnormalities happen by chance and are not typically inherited from a parent or donor. Embryos with aneuploidy are more likely to result in miscarriage or a failed IVF cycle. Less commonly, aneuploidy may result in the birth of a baby with a chromosome condition such as Down syndrome or Turner syndrome.
Preimplantation genetic testing for monogenic disorders (PGT-M): This type of PGT is performed when a patient has an increased risk for a specific genetic condition to occur in his or her embryos. PGT-M is appropriate when an individual is affected with a genetic condition that could be passed on to his or her children, for women who are carriers for an X-linked condition, or when an individual and their partner or donor are both carriers for the same autosomal recessive condition.
Preimplantation genetic testing for structural rearrangements (PGT-SR): This type of PGT is performed when a patient or their partner has a rearrangement of their own chromosomes such as a translocation or inversion. A person with a translocation or inversion is at increased risk to produce embryos with missing or extra pieces of chromosomes. Embryos with missing or extra pieces of chromosomes are more likely to result in miscarriage or a child with serious health issues.
Q: Who should have PGT performed for their embryo(s)?
By contrast, PGT-M and PGT-SR are only performed when the patient, their partner and/or their donor have abnormal genetic test results that put the embryos at increased risk for a genetic disorder. PGT-M is an option for patients with an increased risk for a single gene disorder in their embryos, such as sickle cell anemia. PGT-SR is an option for patients who have a chromosome translocation or inversion. These two procedures allow patients the opportunity to reduce the risk of having an affected child prior to becoming pregnant.
Q: How is PGT performed?
Q: Are there risks to the embryo(s) from the PGT process?
In-House Egg Donation FAQ
Q: How does our egg donation program work?
Q: What are the advantages of utilizing our Egg Donation program?
- As a recipient of egg donation, you will be giving yourself the opportunity to experience all the wonders of motherhood from the very beginning that will allow you to create a lasting bond with your child.
- You and your spouse can carefully choose the characteristics of the donor, which may allow you to find an egg donor whose attributes are very similar to yours.
- You will be giving the fetus an environment that you know and trust for its growth and nurture – your own body!
- It is the closest method available to natural childbearing.
- Very high success rate.
- Egg donation often results in multiple embryos that can be used in the future if you decide to have another child, which makes the entire process a lot shorter and easier for you and your family.
Q; Can we have any contact with our anonymous donor?
Q: How long will this cycle take?
A: This is the million-dollar question. Under normal circumstances if everything goes perfectly, we say it’s about six to eight weeks from contract signing to embryo transfer.
Q: Does the success rate differ by age?
Surrogacy FAQ
Q: What is Surrogacy?
Q: Are there different types of surrogacies?
IVF Surrogacy (gestational carrier)
A woman carries a pregnancy created by the egg and sperm of the genetic couple. The carrier is not genetically related to the child.
Natural Surrogacy (traditional/straight surrogate)
American Reproductive Centers does NOT participate in this type of surrogacy due to California State laws. This is just for information purposes. A woman is inseminated with sperm from the male partners of an infertile couple. The child that results is genetically related to the surrogate and to the male partner but not to the commissioning female partner.
Donor Egg/Gestational Surrogacy
The surrogate agrees to carry the embryos made from the sperm of the intended father and the eggs from a third-party donor. This is commonly used by same-sex male couples to have children.
Q: Why consider surrogacy as a fertility option?
If you are a woman, you may use a surrogate mother because:
- You have uterine issues. The uterus is an incredible organ, but some women have medical roadblocks that prevent them from carrying a baby to full term.
- You have a pre-existing health condition. Beyond uterine issues, other medical conditions can make carrying a baby extremely dangerous – if not life-threatening. Those living with heart and kidney issues, for example, may find surrogacy to be the safest option.
- You have had a hysterectomy. Women who have had cervical or another type of cancer requiring a hysterectomy cannot conceive and carry a child naturally.
- Your previous pregnancies were traumatic. Women who have been pregnant before and experienced serious problems throughout might choose surrogacy to protect themselves and their babies.
Surrogacy is also a popular alternative family planning journey for other couples and individuals, including:
- People that cannot adopt a child because of their marital status or age.
- LGBTQ+ couples that cannot have a child because of logistical reasons. In these instances, surrogacy has several benefits. For example, a gay man can be the biological father of his child.
Q: What are the benefits of surrogacy?
A: There are many benefits awarded to families that have been created in this very special way. These include the following:
- Surrogacy offers the potential for one or two of the intended parents to be related to their child biologically.
- Surrogacy gives parents the opportunity to raise their child from birth.
- The intended parents can be involved in the pregnancy and, in some cases, be present for exciting milestones throughout the journey.
- The intended parents can, if everyone agrees, form a meaningful relationship with the surrogate mother and her family.
- People that peruse surrogacy may face fewer limitations than those that choose adoption.
- The intended parents can rest a little easier when using a surrogate, as the surrogate has undergone extensive medical testing, and many have carried babies to full term in the past. This increases the likelihood of success.
Q: How do I start my surrogacy journey?
A: Our team of surrogacy experts can guide you through every step of the process, offering expert advice on all things medical and legal. Our services are client-tailored, and we can facilitate and oversee surrogacy agreements that use an egg donor, sperm donor, or IVF technologies to help you build the family you’ve always wanted.
We don’t discriminate against different ages, genders, backgrounds, sexual orientations, or marital status. We believe that a world-class surrogacy experience can be life-changing, and whoever you are, we are ready to make your family dreams a reality!
Male & Female Fertility Evaluation FAQ
Q: What does infertility mean? Can I ever have children?
Q: How do we evaluate infertility in women & men?
Most men will initially be diagnosed with a potential male factor fertility issue based on the results of an ejaculated sperm specimen or Semen Evaluation. The components of a Sperm Analysis include:
- Volume
- Sperm Count
- Sperm Motility
- Sperm Morphology
Q: How do you determine what tests to run?
Our fertility testing programs begin by going over the medical history of both partners. This, coupled with a physical exam of both partners helps us to determine what fertility tests to run.
A: The physical exam is both a gynecological exam, a pelvic ultrasound, and a hormone screening for women and a semen analysis on the man. In some cases, a woman also experiences an evaluation of tubal patency. This is used to determine if the fallopian tubes are blocked or not.
Q: How is infertility treated?
A: The most common treatments for infertility are Intrauterine Insemination (IUI) and In Vitro Fertilization. Your ARC specialist will determine and recommend the most effective treatment plan for you.
Q: When should I consider fertility preservation?
A: There is never a wrong time to consider fertility preservation and many reasons to discuss preservation with us. If you are facing a medical condition that may impact your ability to conceive, or if you are not ready to start a family until later in life, it is important to speak with a provider at ARC to see if egg freezing is a good option for you!
Egg Freezing FAQ
Q: What is Egg Freezing?
A: Egg freezing also known as Oocyte Cryopreservation is a method that helps women freeze and store their eggs (oocytes). Women now have the option to stop the “biological clock” from ticking. This treatment option essentially keeps the eggs suspended and prevents the eggs from aging and thereby giving women the ability to delay childbearing.
Currently American Reproductive Centers utilizes the latest methods in egg freezing. In the past previous technologies have made success with egg freezing relatively rare. With the technology that we utilize pregnancy rates are much improved.
Q: What is the best age to freeze my eggs?
A: Ideally, as soon as possible for the best chance of achieving a healthy pregnancy down the road. The reason is, as a woman ages, the number of she owns gets fewer and fewer. Eggs age just like our bodies do. Even if the egg number stays the same as five years ago, their “quality” declines.
Q: Who should consider egg freezing?
A: Egg freezing can be beneficial for a number of reasons for women wishing to preserve their fertility for the future including:
- Women who want or need to delay childbearing in order to pursue educational, career or other personal goals.
- Women diagnosed with cancer.
- Women with objections to storing frozen embryos for religious and/or moral reasons.
Q: How does egg freezing work?
A: Although sperm and embryos have proved easy to freeze, the egg is the largest cell in the human body and contains a large amount of water. When frozen, ice crystals form that can destroy the cell. Our process includes dehydrating the egg and replacing the water with an “anti-freeze” prior to freezing to prevent ice crystal formation. Because the shell of the egg hardens when frozen, sperm must be injected with a needle to fertilize the egg using a standard technique known as ICSI (Intracytoplasmic Sperm Injection). Eggs are frozen using a flash-freezing process known as vitrification.
Q: Is egg freezing expensive?
Elective Single Embryo Transfer (Fresh & Frozen) FAQ
Q: What is Embryo Transfer?
Q: How does the frozen embryo transfer process differ from IVF with fresh embryos?
When PGT-A is performed , all embryos must be frozen at the blastocyst stage after biopsy. ARC does not perform biopsy on cleavage stage embryos but rather on blastocysts.
Q: Who can opt for frozen embryo transfers?
A: ARC works with women between the ages of 18 and 54, offering the fertility treatment that is most appropriate for each patient’s individual circumstances. In general, younger women have higher quality eggs, though of course this is not true in every case. Those who have suffered through multiple miscarriages, endometriosis, or early miscarriage may have different success rates to those who have other infertility issues, and this may be down to the quality of the eggs. However, the earlier a patient visits our center and begins the fertility treatment, the higher the likelihood that her eggs will result in embryos and ultimately result in pregnancy. Any of ARC’s female patients who go through ovarian stimulation are welcome to opt to freeze resulting embryos for future use.
Q: What is ARC’s Embryo Transfer Procedure?
ARC highly promotes elective single embryo transfers.
The embryos chosen for transfer are evaluated by the embryologist and physician to determine the best quality embryos. The number of embryos transferred depends on the patient’s age, history, embryo quality, risk assessment, risk tolerance, and other diagnostic and clinical indicators.
Q: Do frozen or fresh embryo transfers have better success rates?
However, success rates aren’t the only determining factor. Depending on your situation, going fresh over frozen for your embryo transfer may better suit your needs. Let’s explore what to consider when selecting between fresh and frozen embryo transfers during your ARC journey!
Robotic/Advanced Endoscopic Surgery FAQ
Q: What is robotic-assisted surgery?
A: Robotic surgery requires only a minimal incision and places a higher level of precision in the hands of a skilled surgeon. Incredibly accurate 3-dimensional planning facilitates optimal surgical accuracy, often resulting in reduced pain, faster recovery, and improved outcomes.
Q: What are the benefits of robotic-assisted endoscopic surgery?
- Tiny incisions and smaller surgical movements mean less pain
- Shortened hospital stays and mostly outpatient surgeries with same-day discharge.
- Faster road to recovery
- Fewer complications like blood loss and infection
Q: Is robotic-assisted surgery more expensive?
A: Robotic-assisted surgery is typically no more expensive than traditional surgery. And, depending on the specific procedure being performed, it can be far less costly.
Dr. Abdallah is the only Board Certified Reproductive Endocrinologist who uses Robotics.
Media
Dr. Maher Abdallah and American Reproductive Centers in the News!