Coachella Valley’s First & Only Full-Service Fertility Center & IVF Lab
Since 2006, Coachella Valley’s first & only full-service fertility center & IVF lab, American Reproductive Centers’ advanced treatments of infertility have provided our patients with the ultimate gift: the joy of parenthood! Our fellowship trained and board-certified physicians use the latest in world-class assisted reproductive technology in our state-of-the art facilities in Palm Springs & the Coachella Valley to ensure continuity of care beginning with the first consultation through childbirth and graduation to OB/GYN services.
American Reproductive Centers (ARC) SERVICES
Your Journey to Parenthood Begins Here!
In Vitro Fertilization (IVF)
Ranked #1 success rate, etc…
Intrauterine Insemination (IUI)
Competitive rates compared to the national average
Preimplantation Genetic Testing (PGT)
Aneuploidy (A)
Monogenic Disease (M)
Gender Selection
LGBTQ Family Building
Helping LGBTQ Community Build Your Dream Family
Surrogacy
American Reproductive Centers offers In-house surrogacy circumventing the need for surrogacy agencies.
Male & Female Fertility Evaluation
Understanding the Health and Viability of Your Reproductive Organs
In-House Egg Donation
A Good Option for Women with Poor Egg Quality, Advanced Age or a History of Surgery/ Chemotherapy Leading to a Loss of Eggs
Egg Freezing
Preserve Your Ability to Get Pregnant in the Future
Elective Single Embryo Transfer (Fresh & Frozen)
ARC advocates for elective Single Embryo Transfer (eSET).
Robotic/Advanced Endoscopic Surgery
Explore the Options of Minimally Invasive Surgical Procedures to Increase Fertility
Testimonials
Get To Know Us More

Meet Your Doctors
ARC’s Board-Certified Endocrinologists are Your Partners in the Journey to Parenthood!

Start Your Journey With Us
Let’s Explore Your Options Together.
One-on-one

Let’s Answer All Your Questions
You Have Questions, We Have Answers! Check Out our FAQ.
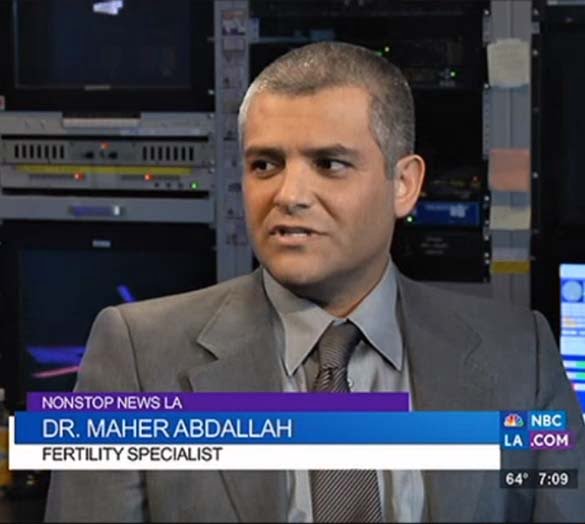
ARC in the Media
We are Making News at ARC! Check Out the Latest!

Where Success is Measured in Heartbeats!
Two Locations:
1199 N. Indian Canyon Dr.
Palm Springs, CA 92262
1-760-346-4334
255 Terracina Blvd. – Suite 202
Redlands, CA 92373
1-760-346-4334